Overview
The Airwayve Podcast is a Canadian anesthesia podcast for medical students led by medical students from McMaster University in Hamilton, Ontario.
As the first of its kind, this podcast aims to make introductory learning about anesthesia concepts accessible, entertaining and succinct. With practical advice for learners, our podcast aims to explore topics in anesthesia by emphasizing cognitive appraisal when approaching unfamiliar content. Recognizing that many students come across anesthesia later in their training, our series also aims to explore anesthesia as a career path and showcase it in different contexts. Content is primarily targeted to medical students, but many episodes will appeal to a broader audience.
Podcasts are released monthly and are meant to help with your introductory learning.
Check out our latest episode!
Core Team
Winnie Liu
3rd year medical student, McMaster University, Writer, Co-Host

Grace Huang
3rd year medical student, McMaster University, Writer, Co-Host
Anna Yang
2nd year medical student, McMaster University, Infographics, Co-Host
Residents

Dr. Puru Panchal
PGY2, University of Toronto,
Founder, Producer, Editor

Dr. Alexa Caldwell
PGY3, University of British Columbia,
Co-Founder, Producer, Editor

Dr. Grace Martin
PGY2, McMaster University,
Co-Founder, Producer, Editor
Faculty
Dr. Daniel Cordovani
MD, MSc
Associate Professor
Director Obstetrical Anesthesia Fellowship

Dr. Daniel Cordovani
MD, MSc
Associate Professor
Director Obstetrical Anesthesia Fellowship
Dr. Amanda Whippey
MD, FRCPC
Assistant Clinical Professor
Program Director UGME Anesthesia Clerkship

Dr. Amanda Whippey
MD, FRCPC
Assistant Clinical Professor
Program Director UGME Anesthesia Clerkship
Dr. Daniel Cordovani
MD, MSc
Associate Professor
Director Obstetrical Anesthesia Fellowship
Dr. Daniel Cordovani
MD, MSc
Associate Professor
Director Obstetrical Anesthesia Fellowship
Dr. Amanda Whippey
MD, FRCPC
Assistant Clinical Professor
Program Director UGME Anesthesia Clerkship
Dr. Amanda Whippey
MD, FRCPC
Assistant Clinical Professor
Program Director UGME Anesthesia Clerkship
Alumni
Thank you to all those who have contributed to the AirWayve Podcast along the way!

Cody Tran, Diljit Gill, James Cho, Emily Au, Karanpreet Bath, Anushka Nair, Amy Ajay, Gwendolyn Lovsted, Dorsia Meng, Maia Shen, Raven Kang
Affiliations

Partnership
This podcast was created in partnership with McMaster University’s Department of Anesthesia.

Support
This podcast was created with generous support from the McMaster University Medical Student Association.
Contact Us
Contact Us Here!
Send an email to get in contact with the Airwayve Podcast team!
Listen Now
 Follow the AirWayve Podcast on Spotify, Apple Podcasts, Instagram and Twitter to stay up to date on the latest episodes!
Follow the AirWayve Podcast on Spotify, Apple Podcasts, Instagram and Twitter to stay up to date on the latest episodes!
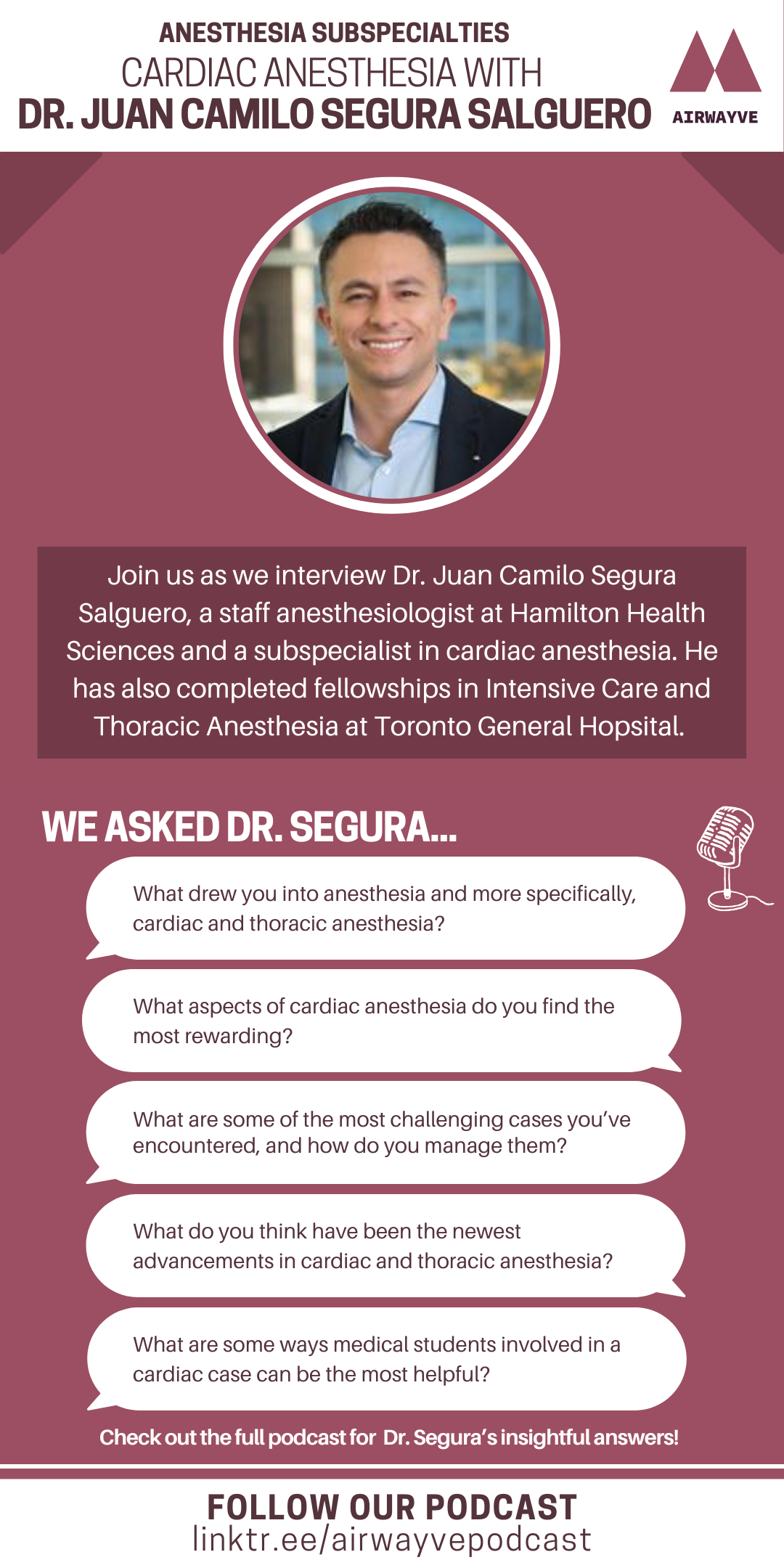
Season 6
Listen to this episode on:
Listen to this episode on:
Listen to this episode on:
Season 5
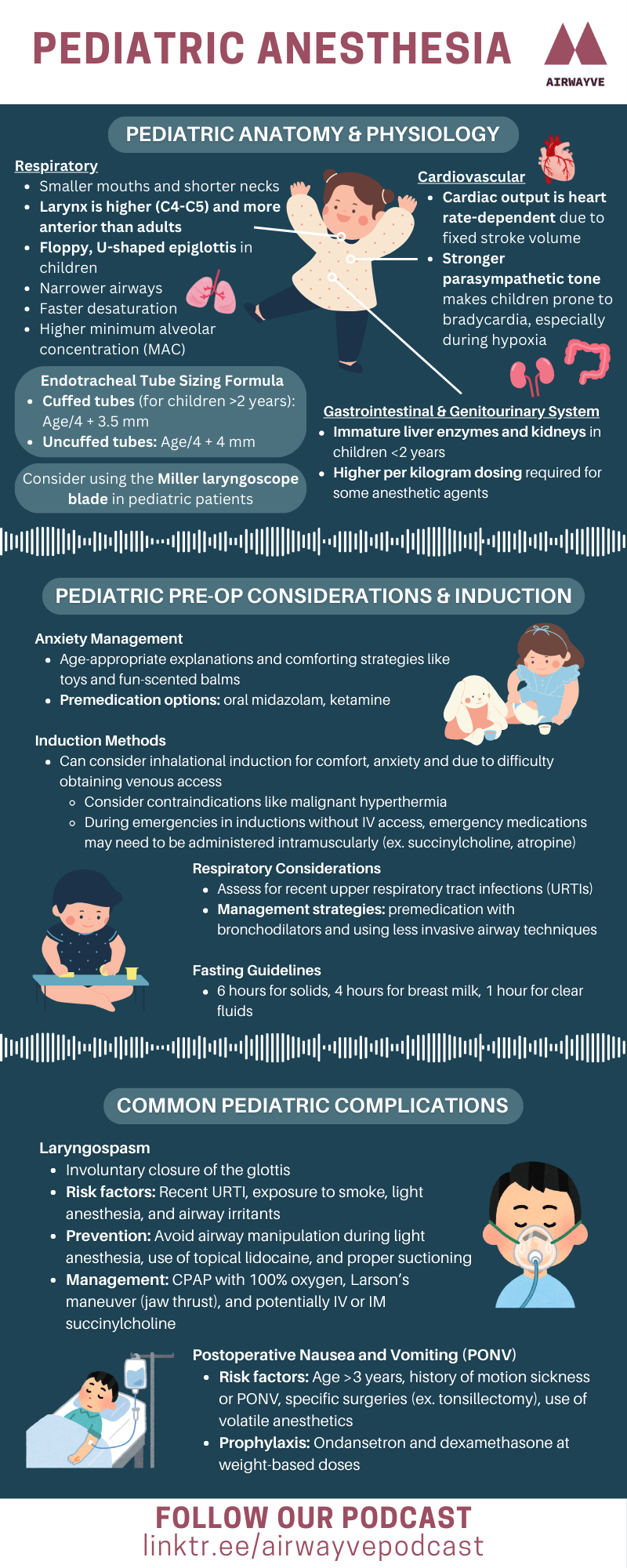
Join two of our new Airwayve hosts Irene and Alex for this month’s episode covering pediatric anesthesia. In today’s talk they give an overview of pediatric anesthesia, including a discussion of anatomy and physiology, preoperative and intraoperative considerations, and common pediatric problems. Remember, kids aren’t just little adults, and this episode gives us a deep dive into why!
Credits:
– Writer: Irene Zhao
– Editor: Winnie Liu, Grace Huang
– Resident Editor: Dr. Grace Martin
– Staff Reviewer: Dr. Amanda Whippey
Listen to this episode on:
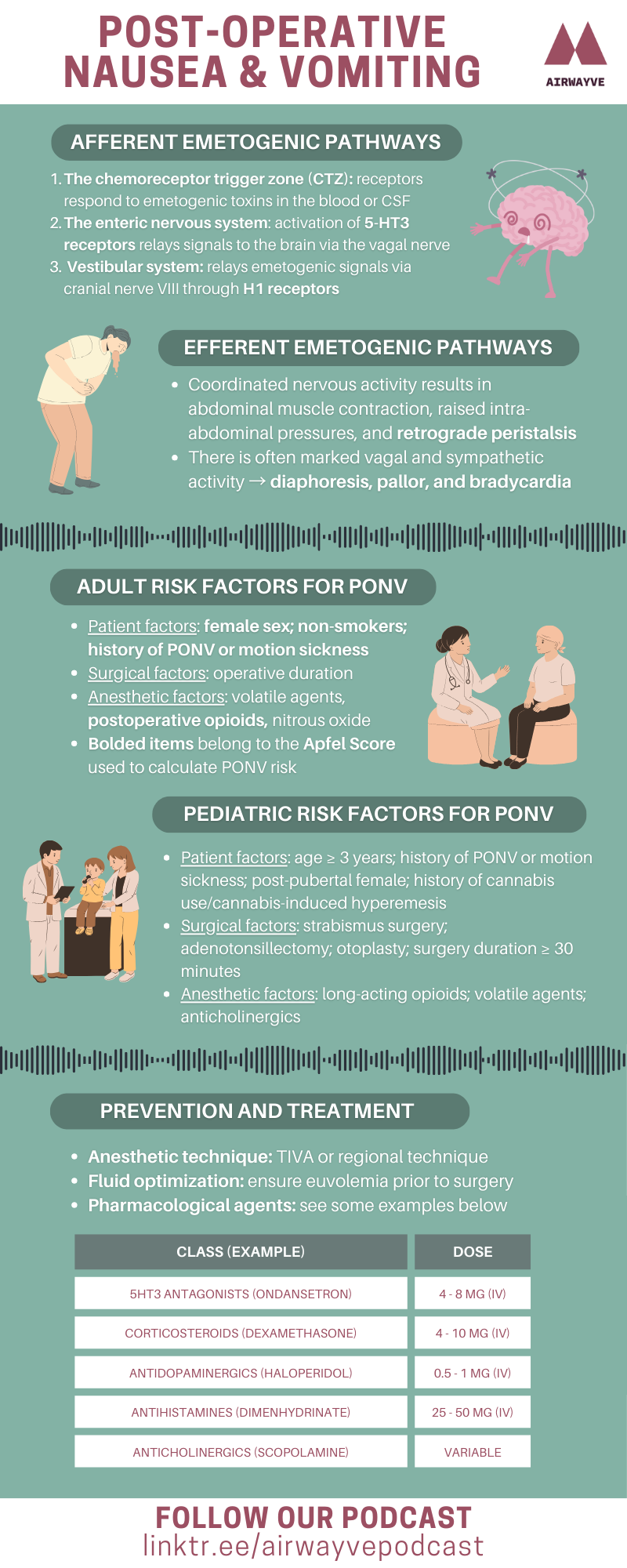
Join Airwayve hosts Winnie and Grace for another episode covering anesthetic considerations. In today’s talk they cover postoperative nausea and vomiting, including the physiology of vomiting, risk factors, and prevention/management. Hopefully this episode doesn’t make you feel queasy!
Credits:
– Writer: Muizz Hussain
– Editor: Raven Kang, Winnie Liu, Grace Huang
– Resident Editor: Dr. Puru Panchal
– Staff Reviewer: Dr. Imran Khan
Listen to this episode on:
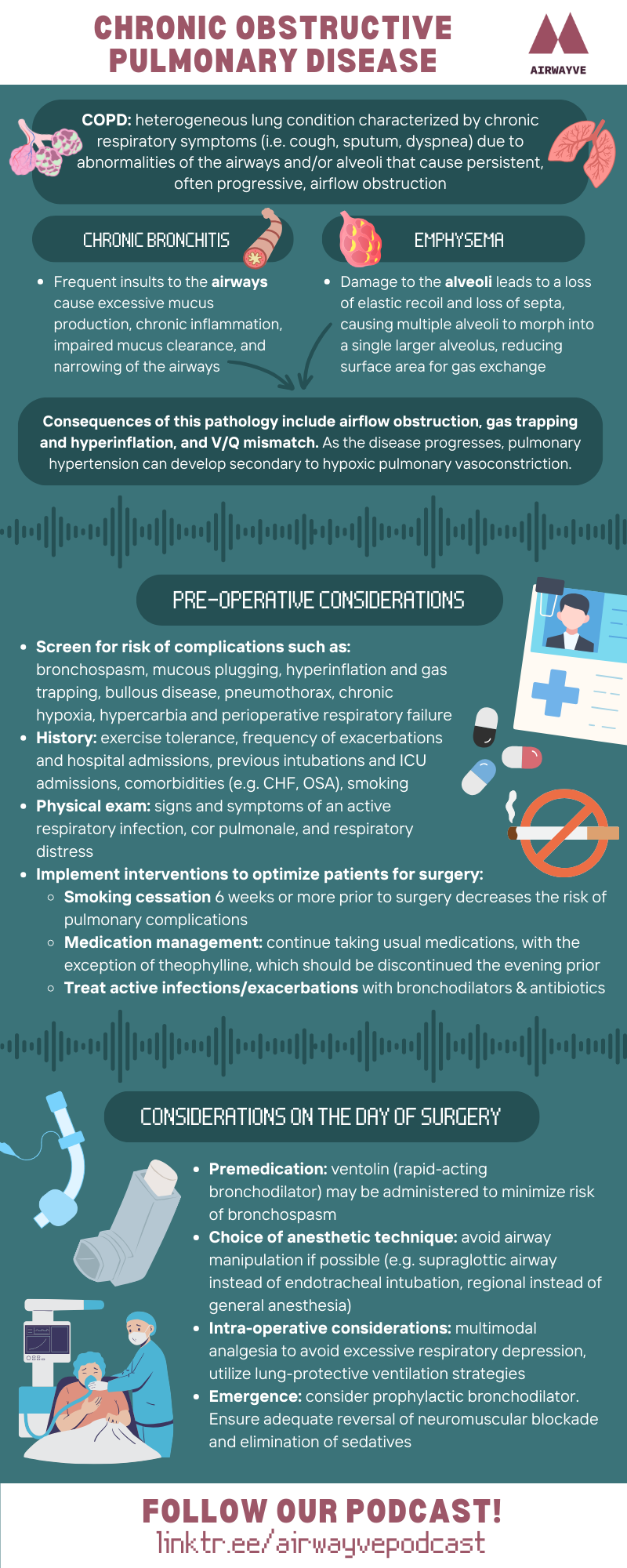
Join Airwayve hosts Winnie and Raven for an episode covering an important concept in respiratory physiology – ventilation and perfusion – as well as anesthetic considerations for patients with chronic obstructive pulmonary disease!
Credits:
– Writer: Winnie Liu
– Editor: Raven Kang
– Resident Editor: Dr. Puru Panchal
– Staff Reviewer: Dr. Andrew Syrett
Listen to this episode on:
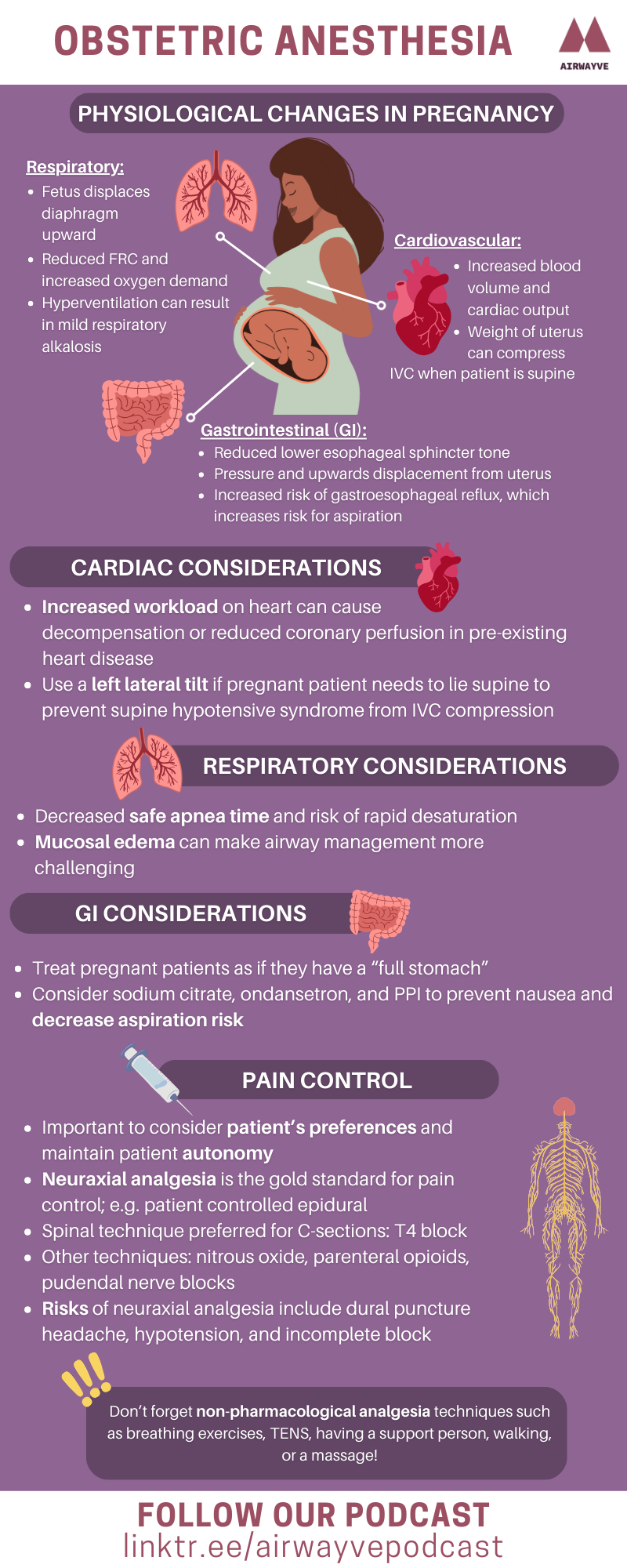
This month’s Airwayve episode is hosted by Dorisa and one of our new hosts, Maxine! We cover some physiologic changes during pregnancy and pre-operative, intra-operative, and post-operative anesthetic considerations for obstetric patients.
Credits:
– Writer: Maxine Maretzki
– Editor: Raven Kang
– Resident Editor: Dr. Grace Martin
– Staff Reviewer: Dr. Annemaria De Tina
Listen to this episode on:
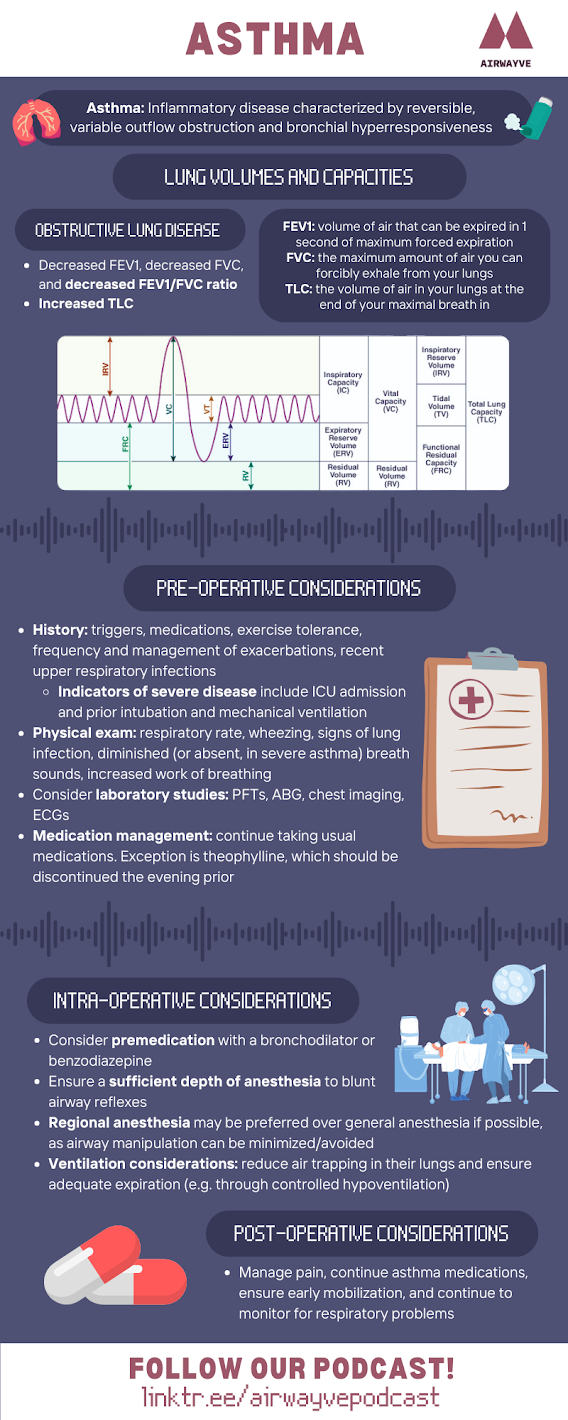
This month’s Airwayve episode is hosted by Maia and one of our new hosts, Winnie! We cover some respiratory physiology, pathophysiological changes in asthma, and finally pre-operative, intra-operative, and post-operative anesthetic considerations for patients with asthma.
Credits:
– Writer: Winnie Liu
– Editor: Raven Kang
– Resident editor: Dr. Puru Panchal
– Staff reviewer: Dr. Anthony Valente
Listen to this episode on:
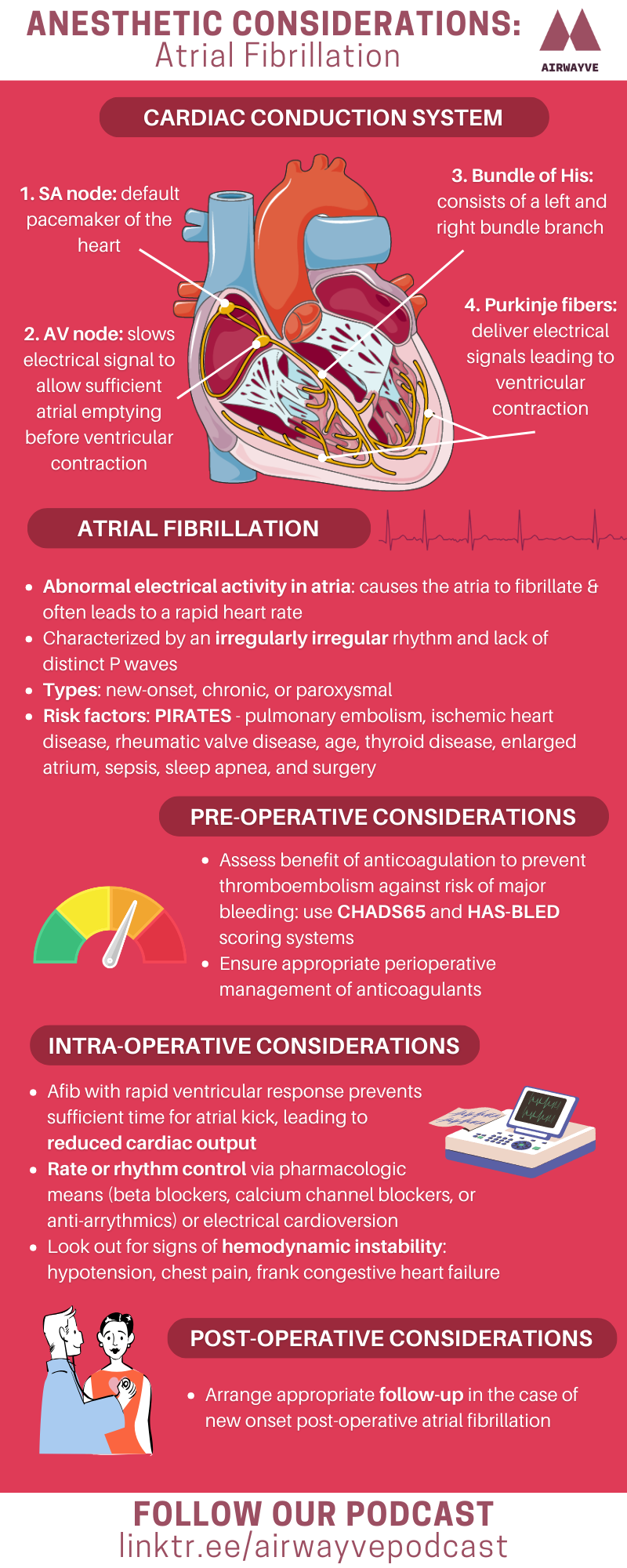
Join Airwayve hosts Raven and Dorisa for an episode on atrial fibrillation. This episode provides an overview of the electrical conduction system of the heart and a brief discussion on the classification of tachyarrhythmias. It also covers pathophysiology, complications, and anesthetic considerations for atrial fibrillation.
Credits:
– Writer: Raven Kang
– Resident editor: Dr. Puru Panchal
– Staff editor: Dr. Mohamad Sharaf Aldeen
Listen to this episode on:
Join Airwayve hosts Raven and Maia for part two of our discussion on diabetes mellitus. In this episode, we cover pharmacology and three life-threatening emergencies: diabetic ketoacidosis, hyperosmolar hyperglycemic state, and hypoglycemia.
Credits
– Writer: Raven Kang
– Resident editor: Dr. Puru Panchal
– Staff editor: Dr. Mohamad Sharaf Aldeen
Listen to this episode on:
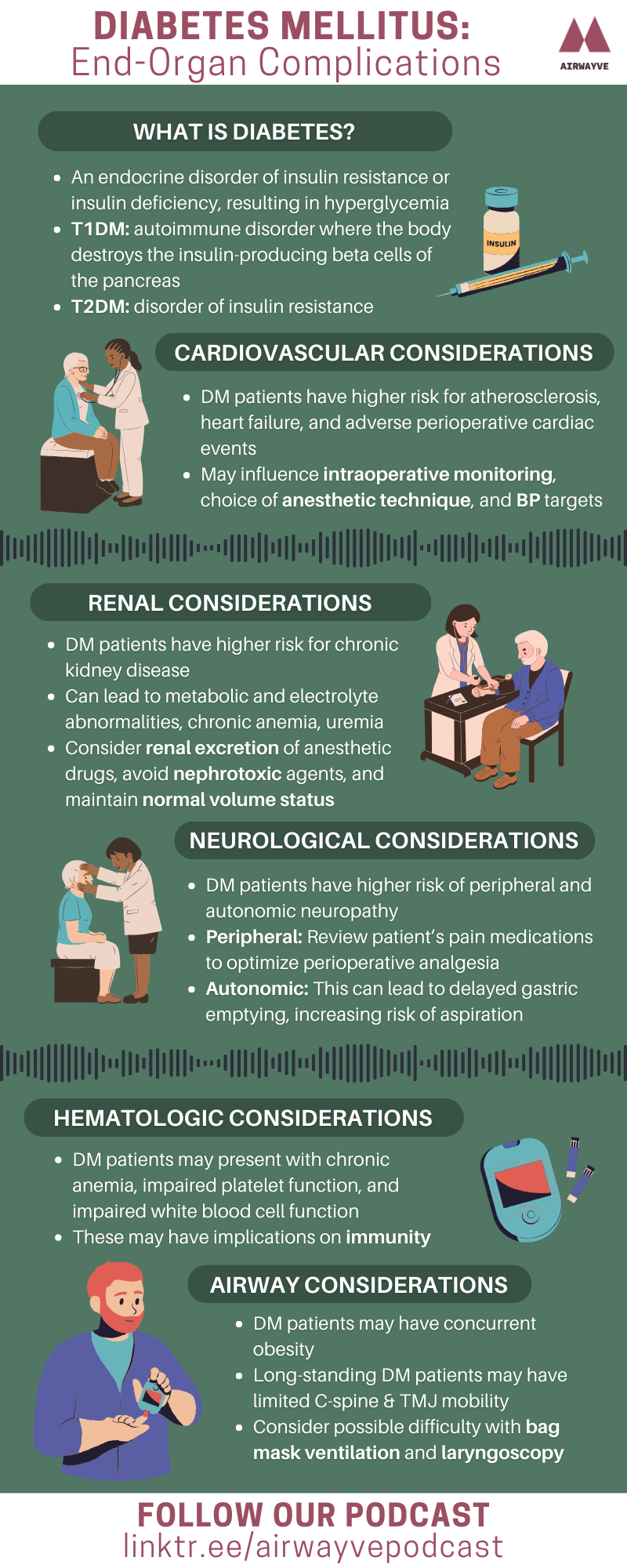
Join Airwayve hosts Raven and Maia for an episode on anesthetic considerations for diabetes mellitus focusing on end organ complications. This episode provides an overview of cardiovascular, renal, neurological, metabolic, endocrine, and airway management implications of diabetes. Stay tuned for the next episode where we cover pharmacology and diabetic emergencies!
Credits
Writer: Raven Kang
Resident editors: Dr. Puru Panchal & Dr. Grace Martin
Staff editor: Dr. Amanda Whippey
Listen to this episode on:
Season 4
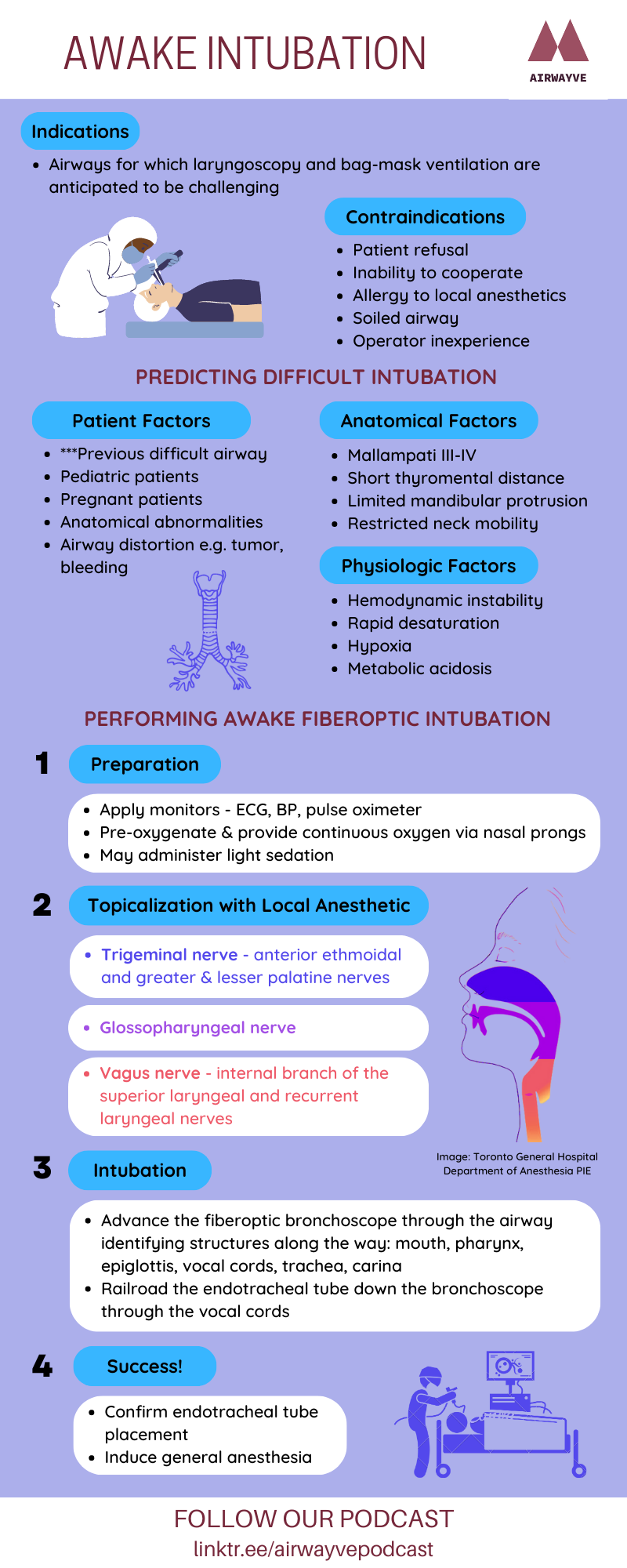
Join Airwayve hosts Raven and Dorisa as they provide an overview of awake intubation covering the following topics, illustrated with a clinical case:
- Review of airway management and indicators of potentially difficult airways
- Indications and contraindications of awake airway management
- Airway anatomy and innervation
- The flexible fiberoptic bronchoscope
Correction: in the podcast episode we use the term “flexible fiberoptic bronchoscope”. A more generic, all encompassing term is “flexible bronchoscope”. The initial technology of flexible bronchoscopes utilized optic fibers (hence, fiberoptic). However, with advancements in technology, most flexible bronchoscopes nowadays have a CMOS (complementary metal-oxide semiconductor, which is a chip that transmits images electronically) camera and light source at the distal tip. This removes the need for optic fibers, which are fragile and expensive to fix.
Credits:
– Writer: Raven Kang
– Resident Editors: Dr. Puru Panchal, Dr. Alexa Caldwell, & Dr. Gabriel Simchovich
Listen to this episode on:
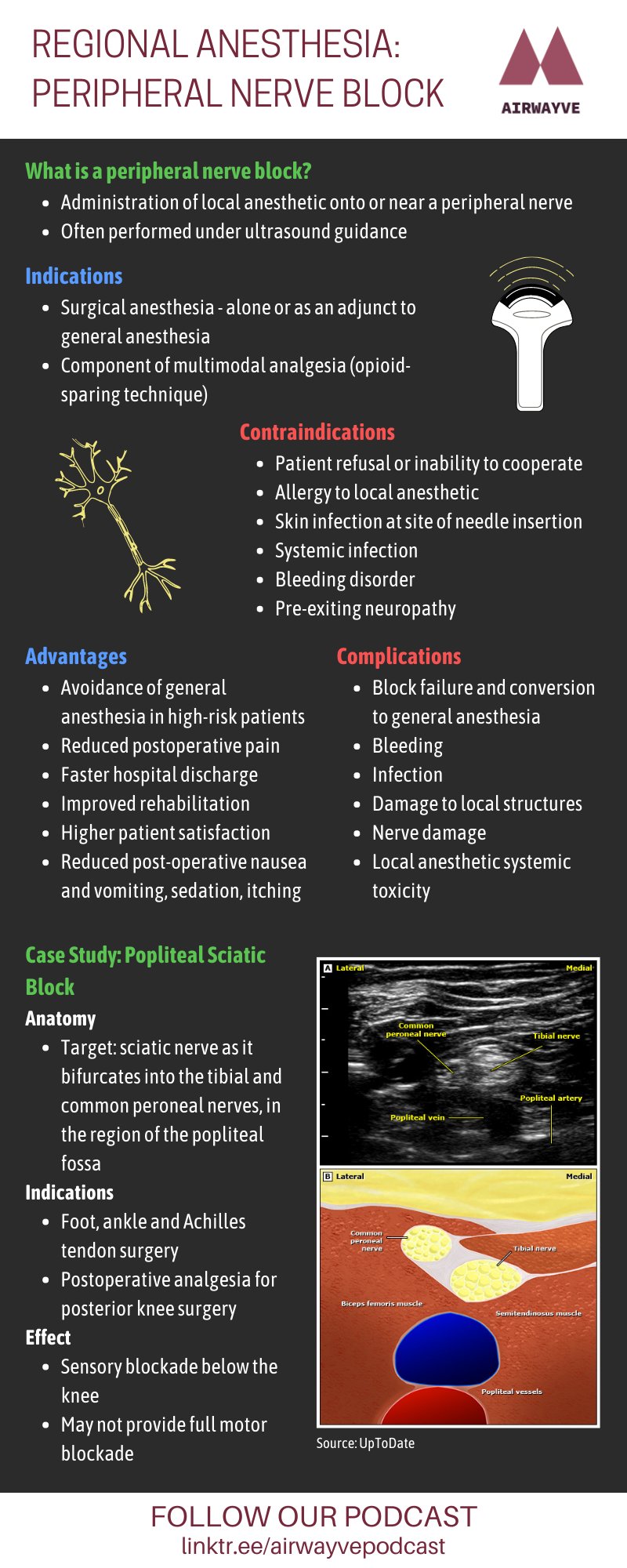
Join Airwayve host’s Maia and Dorisa as they provide an overview of regional anesthesia using a clinical case to cover the following topics:
- What is regional anesthesia?
- An introduction to peripheral nerve blockade
- Indications and contraindications
- An overview of the Popliteal Sciatic nerve block and its relevant anatomy
- What are the techniques involved?
- What are common side effects and adverse events?
Listen to this episode on:
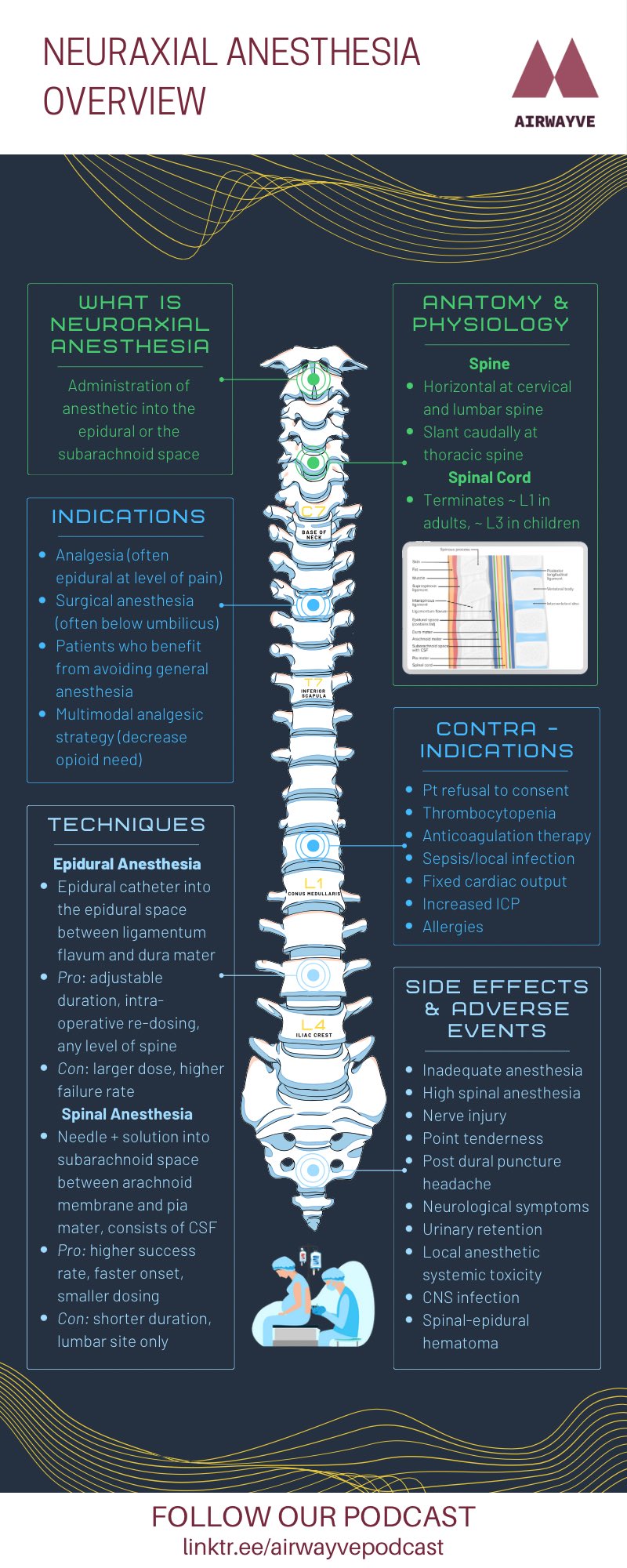
Join Airwayve host’s Diljit and Cody as they provide an in-depth overview of neuraxial anesthesia using a clinical case to answer the following questions:
- What is neuraxial anesthesia?
- What is the relevant anatomy and physiology?
- What are indications and contraindications?
- What are the techniques involved?
- What are the advantages to using this modality?
- What are common side effects and adverse events?
Additional links for more information:
Epidural Information Card
Toronto General Hospital Department of Anesthesia – Spine Anatomy
Listen to this episode on:
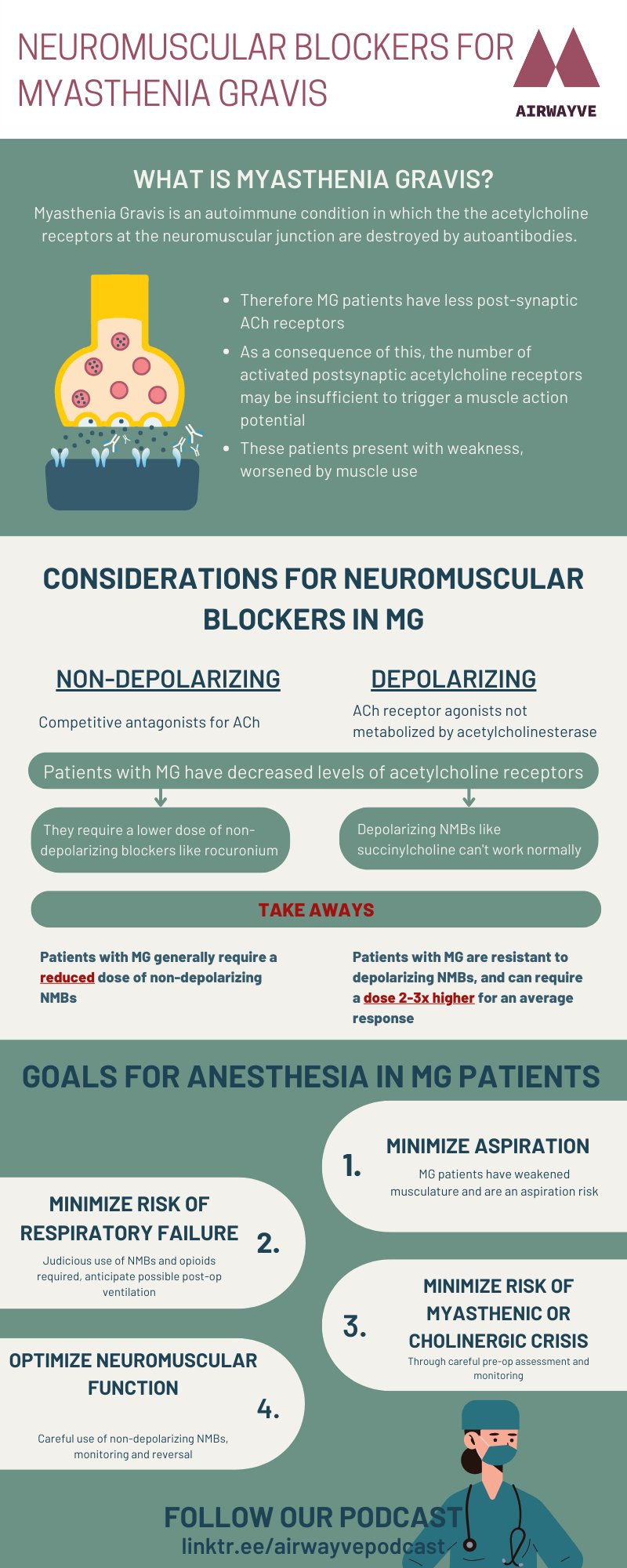
Join Grace and Anushka as they take a deeper dive into the role of neuromuscular blocking agents in the context of patients diagnosed with Myasthenia Gravis. We highly encourage listeners to check out Airwayve S3E2 for a refresher on neuromuscular blocking agents before jumping into today’s action-packed header.
Listen to this episode on:
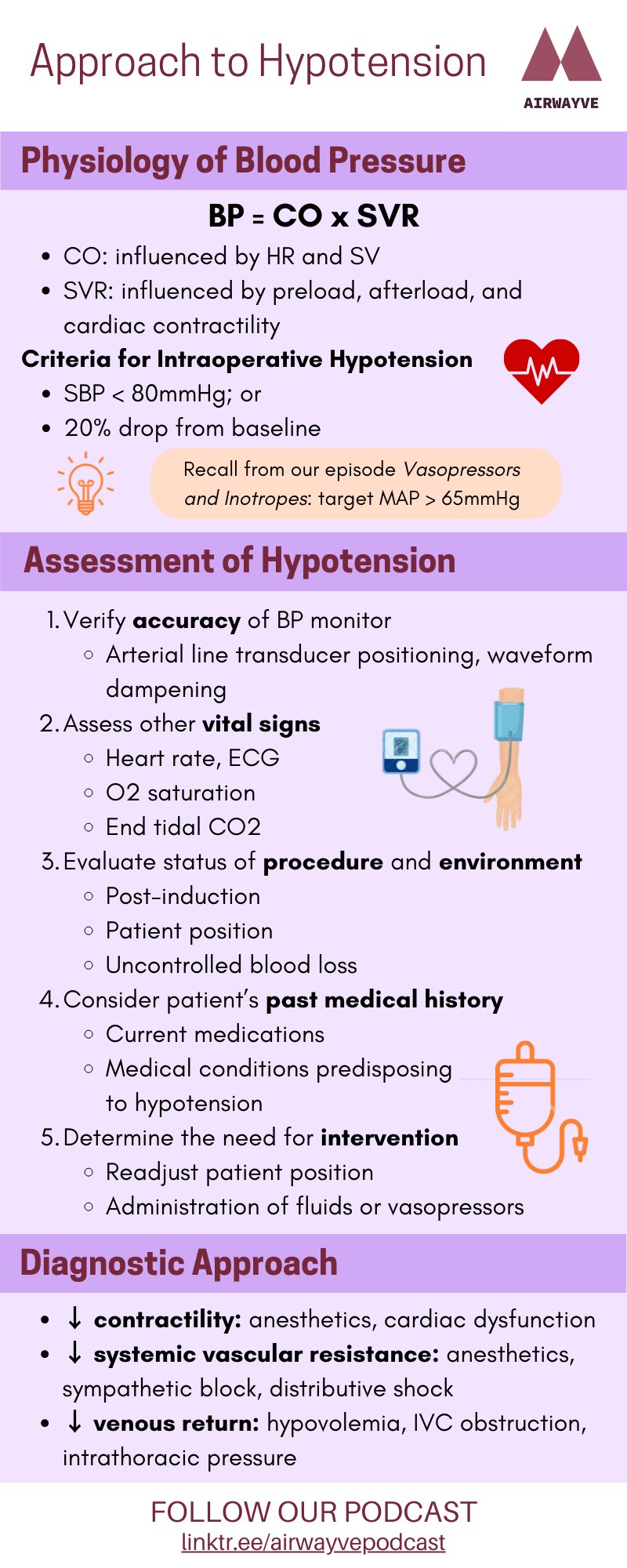
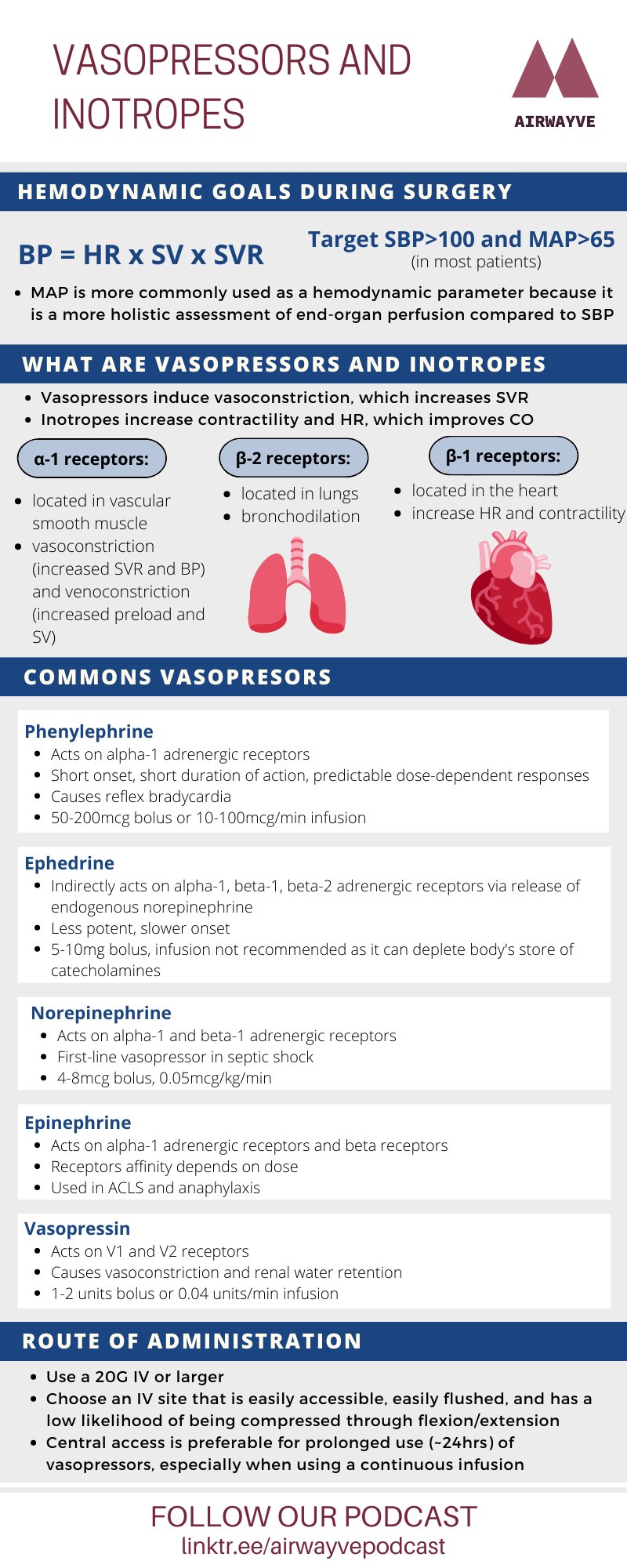
This episode will outline a general approach to understanding, diagnosing, and ultimately managing intra-operative hypotension. Join Airwayve Podcast host’s Diljit Gill and Cody Tran as they provide:
- A review on the physiology of blood pressure
- A general approach to diagnosing and managing intra-operative hypotension
- Applying all of this to a guided clinical case scenario
Credits
Writers: Diljit Gill & Cody Tran
Editors: Diljit Gill & Cody Tran
Resident Editor: Dr. Alexa Caldwell
Staff Editor: Dr. Daniel Cordovani
Listen to this episode on:
Listen to this episode on:
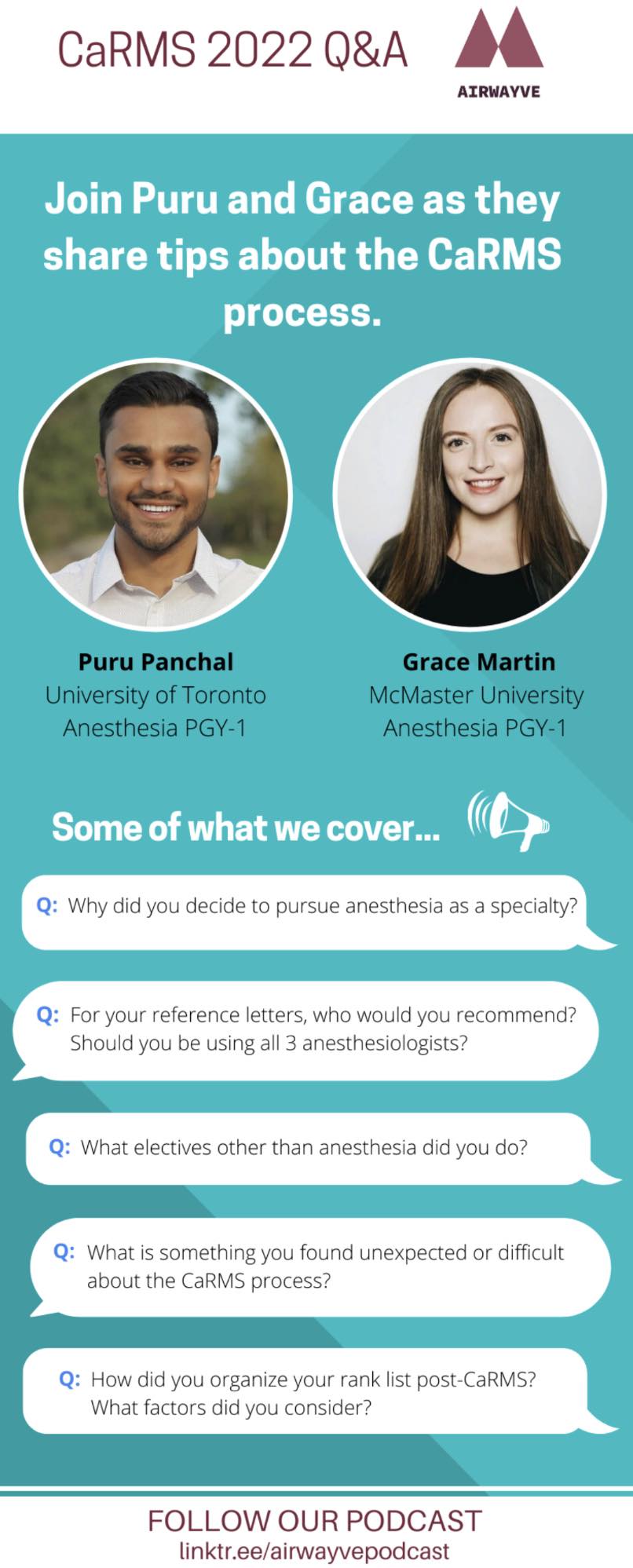
This episode introduces four new Airwayve Podcast hosts Diljit Gill, Cody Tran, James Cho, and Emily Au. Join us as we welcome back former Airwayve hosts and new Anesthesia PGY1’s Dr. Grace Martin and Dr. Puru Panchal for an in depth Q&A style discussion focused on preparing for CaRMS.
Listen to this episode on:
Season 3
Listen to this episode on:
Listen to this episode on:
Dr. Daneilla Dimitri is a Family Practice Anesthetist and Emergency Physician at Stevenson Memorial Hospital and Lakeridge Health. She completed her rural family medicine residency and anesthesia training at McMaster University. She has an interest in crisis management and critical care teaching, especially in the context of rural, resource-limited settings.
Listen to this episode on:
Listen to this episode on:
Listen to this episode on:

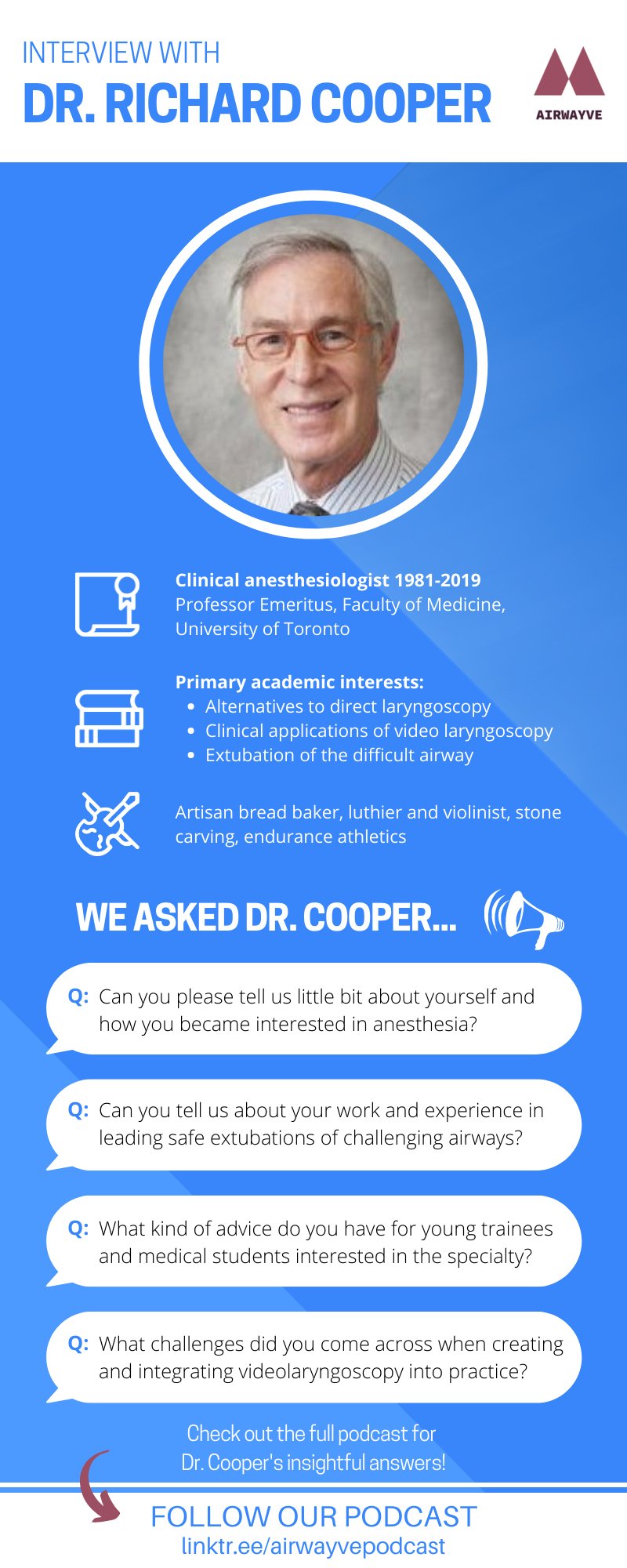
Dr. Cooper a Professor Emeritus in the Faculty of Medicine at the University of Toronto. He spent his career as a Clinical anesthesiologist at University Health Network, Toronto General Hospital from 1981-2019. He was the founder and former Director of the Anesthesia Advanced Airway Fellowship at Toronto General Hospital and the Past President of The Society for Airway Management (SAM) from 2012-14. Join us on this episode as we explore Dr. Cooper’s perspectives and reflections on a successful and rewarding career in anesthesia.
Listen to this episode on:
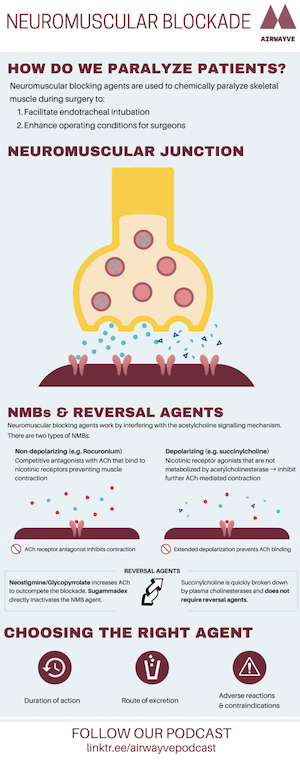
Neuromuscular blocking agents are used to chemically paralyze skeletal muscle during surgery to:
- Provide paralysis of the vocal cords for intubation
- Enhance operating conditions for surgeons
How does skeletal muscle work normally?
An action potential triggers the release of acetylcholine into the neuromuscular junction, which binds to nicotinic receptors on the muscle and causes contraction. As acetylcholine is then degraded, the muscle can begin to respond to stimulation again.
How do neuromuscular blocking agents work?
Neuromuscular blocking agents work by interfering with the acetylcholine signaling mechanism and there are two types:
- Non-depolarizing (e.g. rocuronium): These are competitive antagonists with acetylcholine and bind to nicotinic receptors preventing muscle contraction.
- Depolarizing (e.g. succinylcholine): These act similarly to acetylcholine, as nicotinic receptor agonists, but are not metabolized by acetylcholinesterase and therefore inhibit further acetylcholine-mediated contraction.
How are neuromuscular blocking agents reversed?
- Non-Depolarizing
- Neostigmine/Glycopyrrolate: This method increases the amount of acetylcholine to outcompete the blockade.
- Sugammadex: This method directly inactives the non-depolarizing neuromuscular blocking agent
- Depolarizing
- Quickly broken down by plasma cholinesterases and do not require reversal agents
How to choose a neuromuscular blocking agent? – Questions to consider
- Duration of action
- Are you doing a RSI or not?
- How long do you require skeletal muscle paralysis?
- Route of excretion
- How is the NMB metabolized/excreted and does you patients have any conditions that would prolong the action?
- Adverse reactions and contraindications
- Rocuronium: a common cause of allergic reactions in the OR
- Succinylcholine (the 4 H’s)
- Malignant Hyperthermia
- Hyperkalemia
- High ocular pressure
- Higher post-op muscle pain
Listen to this episode on:
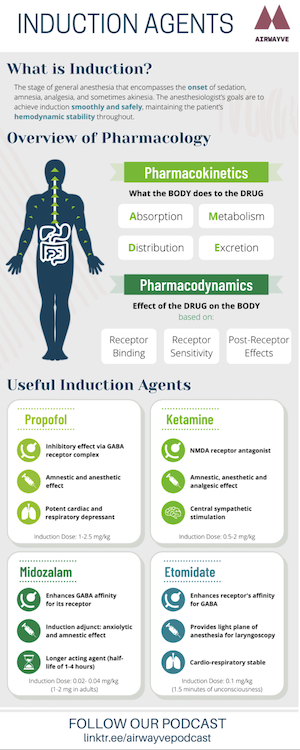
Key principles of pharmacology:
Pharmacokinetics: What the body does to the drug.
A. Absorption
D. Distribution
M. Metabolism
E. Excretion
Pharmacodynamics: A drug’s biochemical and physiologic effects on the body.
- Receptor binding
- Receptor sensitivity
- Post-receptor effects
4 induction agents to familiarize yourself with for the first day in the OR:
1. Propofol
- Inhibitory neurotransmission via the GABA receptor
- Provides reliable amnesia and anesthesia, but does not have any analgesic properties
- Potent cardiac and respiratory depressant
- Easily titratable due to high volume of distribution and short initial distribution half-life
- Induction dose is 1-2.5 mg/kg
2. Ketamine
- NMDA receptor antagonist
- Has analgesic, amnesia and anesthetic properties.
- Can cause emergence delirium
- Causes central sympathetic stimulation
- Induction dose 0.5-2 mg/kg
3. Midazolam
- Enhances the affinity of GABA for its receptor
- Minimal cardiorespiratory depression and produces anxiolysis and anterograde amnesia
- Longer-acting; elimination half-life of 1-4 hours
- Induction doses: 0.02- 0.04 mg/kg (1-2 mg in adults)
- Antagonist available: Flumazenil
4. Etomidate
- Increases the receptor’s affinity for GABA
- Cardio-respiratory stable
- Very fast onset/offset due to high lipophilicity; an induction dose of 0.1 mg/kg will provide 1.5 minutes of unconsciousness
- Produces a light plane of anesthesia for laryngoscopy
- Can cause adrenocortical insufficiency
Listen to this episode on:
Bonus 2021 New Year Episode
Happy New Year! Airwayve is back to bring you tips for your anesthesia rotations. This episode highlights the importance of professionalism in anesthesia and provides 10 practical tips to help you succeed. We thought this episode was quite timely as the second-year medical students at our institution, McMaster University, are beginning their clerkship journey.
Our 10 tips for success are:
1. Be on time or even better be early
2. Introduce yourself to the patient
3. Ask your patients how they pronounce their name, and ask them if it is ok if you call them by it
4. Conclude your interviews by asking patients if they have any questions, or if there is anything that you can do for them
5. Get to know your allied health staff
6. Develop your situational awareness in the OR
7. Be excited to try new things but be aware of the limitations of your technical skills and knowledge
8. Learn more about your preceptor and their preferences
9. Always solicit feedback
10. If you make a mistake, be honest about it, and learn from it.
Listen to this episode on:
Season 2

Dr. Dolores McKeen grew up and did her medical training in Newfoundland. She moved to Halifax to further train at the IWK on a 2-year plan, and ended up staying in Nova Scotia for the last 21 years with her husband Roger, 3 adult children and a senior Yorkie-poo named Miss Molly!
She has conducted research in the areas of post-operative pain management, obstetric anesthesia and health outcomes. Her current research focus is on Patient Centered Care, Knowledge Translation and Implementation of evidence based clinical care such as Enhanced Recovery After Surgery (ERAS). She is the current President of the Canadian Anesthesiologists’ Society (CAS).
Listen to this episode on:
This is the final episode of this series on general anesthesia! PACU handover can seem complicated, but it’s ultimately about transferring professional and care responsibility for your patient after surgery. For this week’s episode, remember the acronym “ISBAR” – as always, check out our step-by-step approach below:
- ID + Introduction: introduce yourself, the surgery team and your patient. This is who YOU are.
- Situation: identify the type of surgery, whether it was elective/urgent, and under what modality of anesthesia your patient just came from (e.g. “John Doe just underwent an elective laparoscopic appendectomy under general anesthesia)
- Background: state your patient’s pertinent medical history and their risks for anxiety, PONV, changes in baseline cognitive status, etc.
- Anesthesia/Actions: mention the technique of anesthesia used and share the patient’s airway features, and if there were any difficulties during the case. This helps the PACU team anticipate problems EARLY! (e.g. “He was difficult to intubate and experienced potential bronchospasm intraoperatively lasting 10 minutes”). Also state the drugs used and their quantities (e.g. “He was given 2mg midazolam, 150mg propofol, 70mcg fentanyl and 10mg ondansetron). Finally, quantify fluids in/out, any pressors/blood products used and their ongoing needs.
- Recommendations: use the PACU order sets to describe what you’d like for your patient (e.g. pain control, PONV medications, IV fluid replacement, hemodynamic management, discharge planning info and when to call the MD for help). (e.g. “We’ve completed the PACU order set and John is expected to return home today. Any questions?”
Listen to this episode on:
What is emergence? The time from discontinuation of an anesthetic to when the patient can make a non-reflex response to verbal command
Maneuvers to improve the elimination of inhaled anesthetics:
- Increase FiO2
- Increase gas flow rate
- Increase PEEP to prevent atelectasis
Factors that affect emergence:
- Patient factors (e.g. obesity, advanced age, hepatic or renal insufficiency)
- Drug factors (e.g. dosage, time of administration, metabolism, excretion)
- Surgical factors (e.g. length/type of surgery)
Reversal of neuromuscular blockade:
- Acetylcholinesterase inhibitor (e.g. neostigmine): increases amount of acetylcholine at the neuromuscular junction to reverse paralysis; also increases acetylcholine in the parasympathetic nervous system
- Muscarinic receptor antagonist (e.g. glycopyrrolate): inhibits the parasympathetic effects of neostigmine
Postoperative considerations:
- Antiemetics: ondansetron, dexamethasone, aprepitant
- Postoperative pain medications: long-acting narcotics, NSAIDs (e.g. ketorolac), acetaminophen
Extubation criteria:
- Hemodynamically stable
- Respiratory rate between 8-35
- Adequate oxygenation (PaO2 at least 60 mmHg with FiO2 <50%, or PaCO2 < 50 mmHg)
- Tidal volume > 5 ml/kg
- Negative inspiratory force of at least 25 mmHg, and vital capacity of 15 mL/kg
- Can also look for purposeful movements such as opening eyes or following commands
Respiratory complications are about 3 times more likely to occur during extubation than intubation
Steps to extubation:
- Deflate the cuff
- Gently remove tube
- Have suction ready, clear secretions prior to extubation and afterwards
- Have oxygenation equipment ready
- Remove monitors from the patient when appropriate (typically remove the oxygen saturation probe last)
Extubation complications:
- Airway obstruction
- Early postoperative hypoxemia
- Heightened cardiovascular response
- Aspiration
- Emergence delirium
Listen to this episode on:
Two overarching goals for the maintenance phase of an anesthetic:
- Maintain appropriate depth of anesthetic
- Maintain patient’s stability
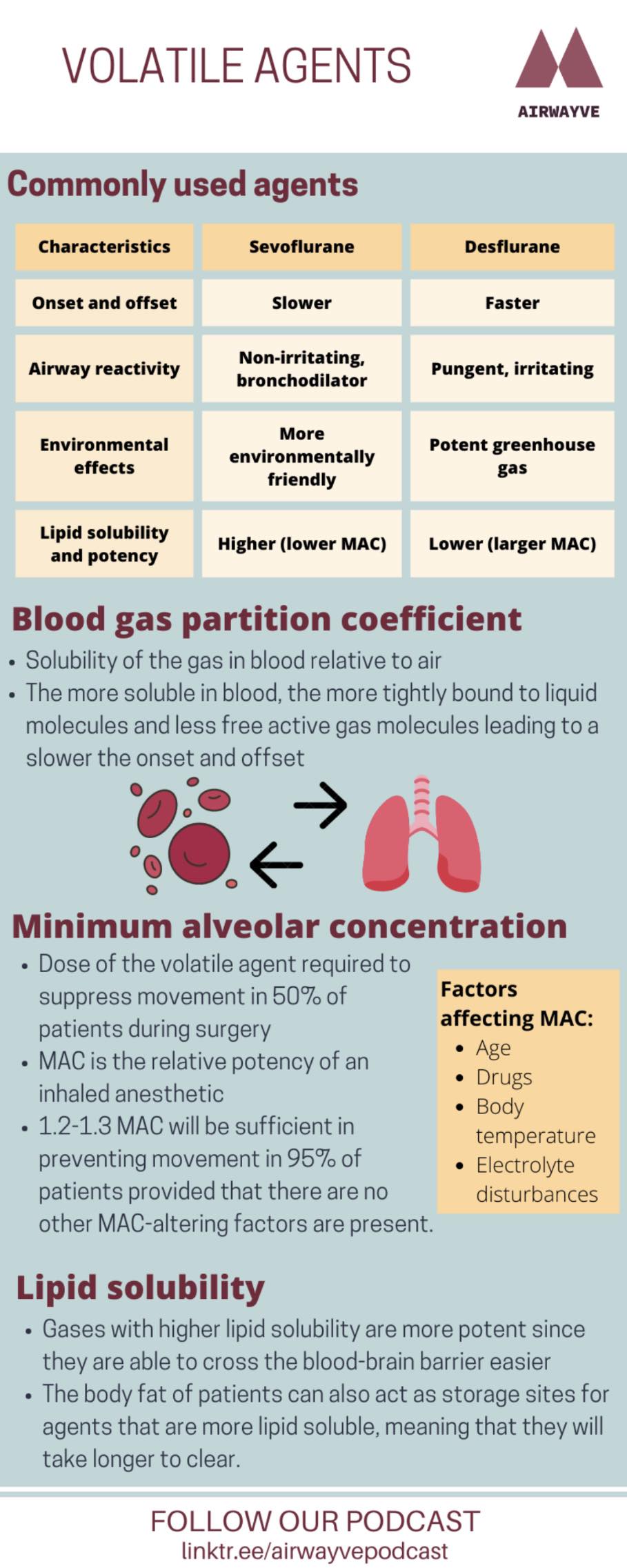
Inhalational Anesthetics
- Volatile agents: sevoflurane and desflurane (most common), isoflurane (less common)
- Nitrous oxide: low potency, can be used in MH, flammable
- Minimum alveolar concentration (MAC): alveolar concentration of a specific inhaled agent that inhibits motor response to a painful stimulus in 50% of patients
IV infusion
- TIVA: total intravenous anesthetic
- Infusion of a sedative agent (most commonly propofol) +/- other agents (such as opioids or benzodiazepines)
- Advantages: can be used in MH cases, less postoperative nausea and vomiting, can avoid airway instrumentation and aerosolization
Intraoperative monitoring
- For each physiologic system, consider:
- What parameters should I be concerned with?
- How can I measure or monitor them?
- What actions can I take to correct an imbalance?
Temperature
- Monitor: temperature probe
- Adjust: air warming device or IV fluid warmer
Neuromuscular
- Monitor: observe patient movement, check Train-of-Four on peripheral nerve stimulator
- Adjust: give neuromuscular blocker if needed, or reversal if appropriate
Ventilation
- Monitor: observe chest rise, auscultate lungs, end-tidal CO2 tracing, flow-volume loop (this goes in the opposite direction with positive pressure ventilation vs. spontaneous breathing!)
- Adjust: ventilator settings such as PEEP, inspiratory pressure, tidal volume, respiratory rate
Oxygenation
- Monitor: observe lips for cyanosis, pulse oximetry on the monitor
- Adjust: FiO2
Hemodynamics
- Monitor: blood pressure, heart rate, ECG tracing
- Adjust: sedative drugs, analgesics, IV fluids; if necessary, consider rescue drugs such as phenylephrine, ephedrine, and atropine
Volume status
- Monitor: blood pressure, intraoperative blood loss, urine output
- Adjust: IV crystalloid fluids, blood products if needed
Practical things to do during the maintenance phase:
- Come to the OR with some questions in mind; the maintenance phase can be a good time to discuss physiology and other concepts with your staff
- Read up on your patient and try to anticipate any specific issues that could arise
- Catch up on charting, if this is done by hand
- Draw up medications for the next case, and ensure that your syringes are organized and labelled
- Go see your next patient and do a preoperative assessment
- Ask your staff, “How can I help?”
Listen to this episode on:
Overall approach to a difficult airway
- Always ask for help!
- The goal is oxygenation, not intubation
- Your first attempt is your best attempt
- Don’t panic!
Preoperative Assessment (check out Episode 1 of the series for a review!)
- Identify risk factors for a potentially difficult airway:
- Difficult ventilation
- Difficult intubation
- Difficulty with patient cooperation/consent
- Difficult cricothyrotomy
- One of the best predictors of a difficult airway is a history of difficult airway
Scenario 1: Can’t intubate, can ventilate
- Return to BMV (bag-mask ventilation) to stabilize the patient and give yourself time
- Try something new with each attempt:
- Switch to a more experienced operator
- Optimize patient position
- Ask an assistant to apply BURP (backwards upwards rightwards pressure)
- Try with different equipment (such as a different size ETT, a Bougie, or videolaryngoscope)
- Minimize the number of attempts (max. 3)
- Consider using a supraglottic airway device or waking the patient up
Scenario 2: Can’t intubate, difficult ventilation
- Improve BMV technique:
- Use an oropharyngeal or nasopharyngeal airway
- Optimize patient position
- Ensure the mask has a tight seal, use 2 hands and ask someone else to bag
- Try inserting a supraglottic airway device
- Once oxygenation is achieved, consider your options for establishing an airway or waking the patient up
Scenario 3: Can’t intubate, can’t oxygenate
- Recognize the problem and communicate with the team
- Proceed with cricothyrotomy / surgical airway
Difficult Airway Society Guidelines
Listen to this episode on:
Check out this great YouTube video which summarizes the steps below: Endotracheal Intubation
Here are a few key steps in airway management:
Ask yourself:
- Will I be able to mask ventilate?
- Will I be able to perform laryngoscopy, directly or indirectly?
- Will I be able to intubate this patient?
- Is there a significant aspiration risk?
History and physical:
- Check your patients’ anesthetic history for any record of a previously difficult airway.
- Difficult bag-mask – BONES: beard, obesity, no teeth, elderly, snoring (or OSA)
- Mouth opening & Mallampati score (high score = difficult laryngoscopy!)
- Thyromental distance (see below) and sternomental distance
- Mobility at the temporomandibular joint and prognathism
Managing the airway:
- Pre-oxygenate patient to end-tidal O2 of >80%
- Align the oral/pharyngeal/laryngeal axes via the “sniffing position”
- Helpful tip! Place folded sheets, rolled blankets or a foam headrest underneath patients’ neck to help achieve this position.
- Hold your Mac blade in your left hand; advance the blade to the vallecula while sweeping the tongue out of the way
- Apply pressure up to the corner of where the wall/ceiling meet to reveal the glottic opening and visualize the cords
- Describe the view of the cords using the Cormack-Lehane scale! If you can’t see the cords, use the BURP maneuver
- Stop advancing the tube when you see the proximal end of the endotracheal tube is at 21-22 cm at the front teeth in an adult – then ask for the cuff to be inflated
Confirm tube placement:
- Auscultate for breath sounds
- Check capnography
- Look for symmetric rise and fall
- Celebrate with a little happy dance (in your head)
Listen to this episode on:
In this episode, we discuss induction, the stage of general anesthesia that encompasses the onset of sedation, amnesia, analgesia, and sometimes akinesia. The anesthesiologist’s goals are to achieve induction smoothly and safely, maintaining the patient’s hemodynamic stability throughout.
Step 1: Place monitors on patient (see Episode 2 show notes for a list of the CAS’ required monitors).
*Clinical Tip: Take a moment to double-check that all monitors are attached to the patient and showing up correctly on the screen. Run some fluids through the patient’s IV for a few seconds to check that it is functioning reliably.
Step 2: Surgical timeout.
*Clinical Tip: The patient needs to be awake for this step, so hold off on giving any sedatives or psychoactive medications until after the timeout.
Step 3: Pre-oxygenation.
*Clinical Tip: Aim for an end-tidal oxygen concentration (EtO2) of >0.8.
Step 4: Administer induction agents (intravenous or inhalational, depending on the type of induction). Typical IV induction agents may include an opioid, a benzodiazepine, an induction agent (sedative), and a neuromuscular blocker.
*Clinical Tip: Propofol and some other induction agents can cause hypotension, so keep an eye on the patient’s blood pressure readings after administering your medications.
Step 5: Assess the depth of anesthesia before proceeding with airway management.
*Clinical Tip: You can check the orbicularis oculi reflex by lightly brushing the patient’s eyelashes with your finger.
Canadian Anesthesiologists’ Society (CAS) Guidelines (2020)
Listen to this episode on:
In this episode, we discuss setting up the operating room for a general anesthetic. The mnemonic SOAP-IM(S) is a helpful checklist for organizing all of the necessary equipment.
1. Suction
- Is the suction equipment (Yankauer/suction system) present and working?
2. Oxygen:
- Check circuit tubing, gas analyzer tubing, filter, face mask
- Check for availability of back-up O2 tank
3. Airway:
- Have a plan for potentially difficult airways (stay tuned for the next episode!)
- Prepare an appropriately sized endotracheal tube (ETT), laryngoscope & oropharyngeal/nasopharyngeal airway
- Check ETT cuff for leaks
- Have backup equipment ready
- Know where to access video-laryngoscope
4. Pharmacy:
- Check for commonly used medications and rescue medications
- Check the expiry dates of medications as you draw them up, and label each syringe with the medication and concentration
5. IV: equipment for placing an IV, fluids, IV tubing.
6. Machine: anesthetic machine check.
- Check for leaks
- Ensure circuit can supply positive pressure
7. Monitors: refer to the CAS requirements
- Standard required monitors for every patient:
- Pulse oximeter
- Blood pressure (NIBP)
- 3-lead or 5-lead ECG
- ETCO2 gas analyzer – measure of ventilation
- Other equipment you will commonly use:
- Capnography
- Temp monitor
- Stethoscope
- Peripheral nerve stimulator
8. Special equipment + Seat: any extra case-specific equipment, and chairs for you and your staff!
- Consider special equipment such as blood products as needed
Listen to this episode on:
This is the first episode in series #2 (approach to general anesthesia). In this episode, we break down the pre-operative evaluation.
Step 1: Confirm patient identifiers and NPO status
Step 2: Focused anesthetic history
- Review of systems: CV, resp, GI, GU, neuro (Bonus: endo)
- PmHx/PsHx with previous surgical complications – always ask about pseudocholinesterase deficiency and malignant hyperthermia
- Meds/allergies and compliance to medication
Step 3: Focused physical exam
- Airway assessment
- BONES mnemonic + Mallampati score
- Mouth open
- Thyromental distance
- Protrude mandible and bite upper lip
- Neck extension/flexion
- CV exam
- Resp exam
- (Neuro exam if indicated)
- ASA status
Step 4: Discuss risks and obtain informed consent
- Risk to teeth: 1/1000
- Typical risks: postoperative pain, postoperative nausea/vomiting, sore throat
For a more detailed description of the modalities of anesthesia and their indications, refer to Chapter 3 of the Ottawa Anesthesia Primer
Patterson L. Ottawa Anesthesia Primer: Patrick Sullivan. University of Ottawa, Faculty of Medicine. ECHO Book Publishing, 2012. ISBN 978-0-9918009-0-2. Can J Anesth Can d’anesthésie 2013. https://doi.org/10.1007/s12630-013-9997-4
Listen to this episode on:
Season 1
 Dr. John Centofanti is an Assistant Professor in the Department of Anesthesia and Program Director of the Critical Care Residency Program McMaster University. He is also a critical care physician and anesthesiologist in Hamilton, Ontario. Join us as we ask about his unique experiences in training and his insights into a career in anesthesiology.
Dr. John Centofanti is an Assistant Professor in the Department of Anesthesia and Program Director of the Critical Care Residency Program McMaster University. He is also a critical care physician and anesthesiologist in Hamilton, Ontario. Join us as we ask about his unique experiences in training and his insights into a career in anesthesiology.
Listen to this episode on:
In this episode, we discuss the diverse roles that anesthesiologists have in the hospital and outpatient settings and tackle some stereotypes and myths about the specialty.
Anesthesiologists can be seen in:
- The operating room and pre-op clinics
- ICU
- ER
- Labour and delivery
- On the wards as part of the Acute Pain Service (APS)
- In chronic pain clinics
Common myths:
- Anesthesiologists do the same things each day
- Anesthesia is only about putting people to sleep
- It’s “boring” work
- Anesthesiologists don’t diagnose conditions
Check out this article written by a McMaster Med student which discusses how anesthesia is portrayed on TV:
Mostly unseen on the television screen
Listen to this episode on:
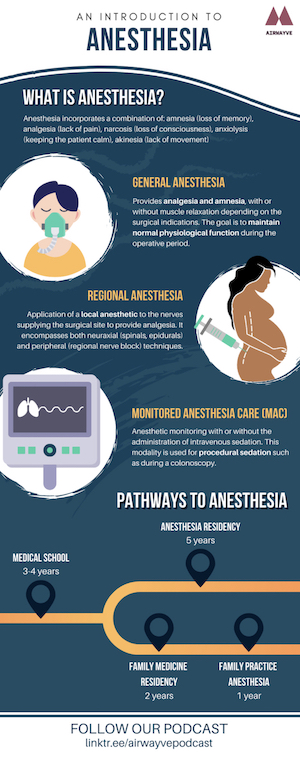
In this episode, we provide a brief overview of our podcast, and the general modalities of anesthesia. These encompass:
- General Anesthesia: Provides analgesia and amnesia, with or without muscle relaxation depending on the surgical indications. The goal is to maintain normal physiological function during the operative period.
- Regional Anesthesia: Application of a local anesthetic to the nerves supplying the surgical site to provide analgesia. It encompasses both neuraxial (spinals, epidurals) and peripheral (regional nerve block) techniques.
- Monitored Anesthesia Care: Anesthetic monitoring with or without the administration of intravenous sedation. This modality if used for procedural sedation such as during a colonoscopy.
For a more detailed description of the modalities of anesthesia and their indications, refer to chapter 2 of the Ottawa anesthesia Primer
Patterson L. Ottawa Anesthesia Primer: Patrick Sullivan. University of Ottawa, Faculty of Medicine. ECHO Book Publishing, 2012. ISBN 978-0-9918009-0-2. Can J Anesth Can d’anesthésie 2013. https://doi.org/10.1007/s12630-013-9997-4
Listen to this episode on: